Blepharitis Treatment
The Ultimate Guide
What Are The Symptoms,Causes,Treatment & Cures For Blepharitis
The Ultimate Guide
To Blepharitis
Symptoms,Causes,
Treatment & Cures
All you ever wanted to know and more
You’re probably here because you want to know more about blepharitis treatment.
If you have already done some research, you may have heard that there is no way to cure blepharitis. I am sure you also found a lot of contradictory information on what causes blepharitis and how to treat it.
To find a blepharitis cure I spent years researching and testing to get the real answers we all need.
Below I take you through everything I’ve learned about blepharitis treatments and causes, Step by Step. Reading this will help you understand what caused your blepharitis and how to treat it.
CHAPTER 1:
What Is Blepharitis
Blepharitis is a term for inflammation of the eyelids. It is one of the most common eye diseases diagnosed by eye doctors.
Unfortunately the question what is blepharitis? does not have a simple answer.
Blepharitis comes in two basic forms Anterior Blepharitis and Posterior Blepharitis. Bacterial infections or other skin conditions may also be present.
Blepharitis that only affects the outside of your eyelids, is Anterior Blepharitis. The symptoms are flaky skin on your eyelids and around your eyelashes. This is usually accompanied by redness and a stinging or burning sensations in your eyes.
The other main form of Blepharitis is Posterior Blepharitis. In Posterior Blepharitis, the problem is in the glands that lubricate your eyes.
Both types can vary in severity and a combination of both is quite common.
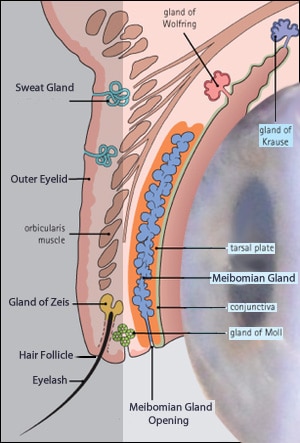 Here is a “Road map” of the affected areas .
Here is a “Road map” of the affected areas .
The main items are in heavier type.
The darkened area on the left is the Anterior section of the eye.
The area on the right is the Posterior section of the eye.
Anterior Blepharitis
 Seborrheic Blepharitis also called Squamous Blepharitis is another form of Anterior Blepharitis.
Seborrheic Blepharitis also called Squamous Blepharitis is another form of Anterior Blepharitis. The Glands of Zeis are sebaceous glands that service your eyelashes. Seborrheic Blepharitis can occur when these glands are malfunctioning. Excessive oil or change in quality produces an oily coating that forms crusts, or scales on the skin.
Posterior Blepharitis
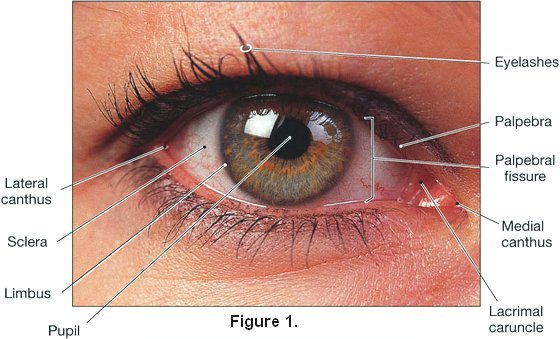
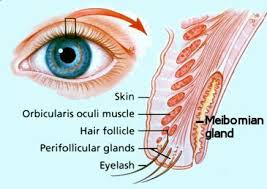
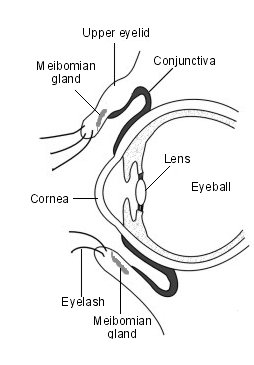 Posterior Blepharitis refers to inflammation of the inner surface of the eyelid. The diagram at Figure 3 is included to show you the glands and tissue at the back (posterior) surface of your eyelid that are affected in Posterior Blepharitis. The a
Posterior Blepharitis refers to inflammation of the inner surface of the eyelid. The diagram at Figure 3 is included to show you the glands and tissue at the back (posterior) surface of your eyelid that are affected in Posterior Blepharitis. The a
rea includes all the inner surface, the Conjunctiva and Meibomian glands and extends to the edge of the outer angle of the eyelid.
Your Meibomian Glands are a specialised sebaceous gland at the rim of your eyelids responsible for the supply of meibum, an oily substance that prevents evaporation of the eye’s tear film.
Much of the available information is a little confusing as often Meibomian Gland Dysfunction (MGD) and Posterior Blepharitis are used interchangeably, and this is not necessarily the case.
Posterior blepharitis is a term used to describe inflammatory conditions of the posterior lid margin of which MGD is only one cause. Other causes include infectious or allergic conjunctivitis and systemic conditions such as acne rosacea. In some respects this is a case of which came first the chicken or the egg.
Can anterior blepharitis lead to posterior blepharitis, conjunctivitis or MGD? Quite possibly. As with many health issues, if a minor problem is not addressed it can often lead to a more serious disorder or disease further down the road.
We will discuss Anterior Blepharitis, Posterior Blepharitis and Meibomian Gland Dysfunction in more detail in the next Chapter on causes.
CHAPTER 2:
What Causes Blepharitis?
How did I get Blepharitis? Is Blepharitis contagious? How long does Blepharitis last?
When there is something wrong with us it is natural to want a simple answer about what caused it. Unfortunately there is no one simple answer.
In this chapter we will look at some of the factors associated with blepharitis. The aim here is that you can identify and correct some of those factors that have led to your current condition.
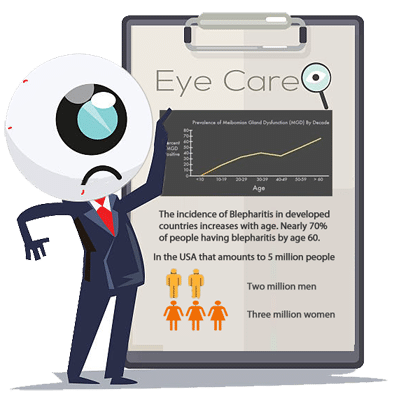
Blepharitis can affect people of any age but the older we are the greater our chance of developing it. The average age of people afflicted with chronic blepharitis is 50 years old. Yet if we look a little closer, around the 40 year old mark there are 30% more women with blepharitis than men.
Blepharitis Causes In Your Environment
Poor Eyelid Hygiene, Now don’t take offence here, I am not suggesting that you don’t wash. However most of us particularly men splash a bit of water on our face, maybe with a little soap or not, a quick rinse and you’re are done. What we don’t realise is that the protective hollow that nature has built for our eyes using the cheekbone, nose and brow ridge also stops the usual quick face wash from cleaning our eyelids and lashes. The prevention and cure for all forms of blepharitis begins with good eyelid hygiene. More about this later.
Occupational factors such a dirty or dry dusty working conditions, allergies and eyestrain while not necessarily causing blepharitis, they can provide the conditions for blepharitis to develop. For example a dusty environment may cause you to rub your eyes and scratch the soft membranes surrounding your eyes and opening them to infection. As you would expect, there is a greater incidence of Blepharitis and Dry Eye in populations living in a dry and dusty climate.
Computer Eyestrain This one is a double hit.  Aside from the glare and lack of focal variation, it has been found that when a person is concentrating on a computer screen their blink rate can be significantly reduced. This reduction in blink rate can lead to dry eyes and potentially to dry eye syndrome which is absolutely linked with posterior blepharitis and/or Meibomian Gland Dysfunction.
Aside from the glare and lack of focal variation, it has been found that when a person is concentrating on a computer screen their blink rate can be significantly reduced. This reduction in blink rate can lead to dry eyes and potentially to dry eye syndrome which is absolutely linked with posterior blepharitis and/or Meibomian Gland Dysfunction.
Contact Lenses. If you wear contact lenses then I am sure you can remember when dust, someone smoking or leaving a lens in for too long has given you sore red eyes which if it happens frequently can lead to blepharitis. Poor contact lens hygiene is another risk factor which has been linked to blepharitis and treatment can often necessitate not wearing contacts for a period of time until symptoms are brought under control.
Makeup. While blepharitis is generally not regarded as contagious there are some exceptions. An acute staphylococcal infection can set you up for chronic blepharitis. As I mentioned in introducing this chapter, there is such a massive difference in the incidence of staphylococcal induced blepharitis between men and women that you could say it is almost a predominantly female condition. The culprit is eye makeup and how it is handled so the answer to this one is in your hands. Eye makeup, eyewashes and eye creams can be a great breeding ground for bacteria. For further information go to staphylococcal blepharitis and makeup – prevention and cure.
Seborrheic Blepharitis.
Fungal and Yeast Infections can also lead to seborrheic blepharitis with the accompanying flaking and scaling of the skin including eyelids.
can also lead to seborrheic blepharitis with the accompanying flaking and scaling of the skin including eyelids.
This often begins as a general skin condition in adults with the development of severe dandruff and rashes on upper parts of the body and face.
The yeast bacterial strain called Malassezia furfur which thrives in the oil of human skin without causing harm to most people is often implicated in an outbreak when a person’s health and immune system is not in good shape.
Now we come to some of the creepier stuff… and things that could be “bugging” you.
Demodex Blepharitis
 Our bodies, inside and out, are home to a huge variety of microscopic creatures. Many of these microbes & bacteria are beneficial, a few can be harmful. Scientists are discovering how important many of these microbes are to our health.
Our bodies, inside and out, are home to a huge variety of microscopic creatures. Many of these microbes & bacteria are beneficial, a few can be harmful. Scientists are discovering how important many of these microbes are to our health. 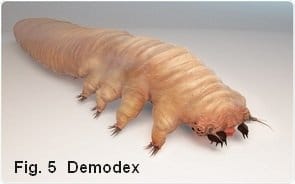 Any way you cut it you don’t want them so one of our tasks is to get rid of them.
Any way you cut it you don’t want them so one of our tasks is to get rid of them.This brings us to the next and often major issue, Meibomian Gland Dysfunction.
Meibomian Gland Dysfunction or Disease?
Carrying on from the above discussion on Demodex Mites we now need to consider whether Meibomian Gland Dysfunction (MGD) is a cause or a symptom of Demodex infestation.
More than 60% of people suffering with MGD also have a demodex infestation so demodex is a likely cause. However that leaves many cases of MGD without excessive numbers of demodex so there are obviously other causes. Before we get into the detail there is another distinction it is important to note.
You may have noticed that I have used the terms Meibomian Gland Dysfunction and Meibomian Gland Disease. Without going into too much detail “Disease” in this case is a broader term and can refer to many different conditions that affect the Meibomian glands such as staphylococcal and fungal infections, neoplasia (tumour or abnormal cell growth), congenital defects or abnormalities that may or may not cause the sebaceous glands to malfunction.
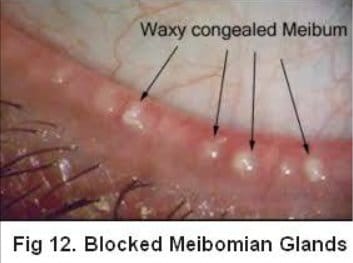
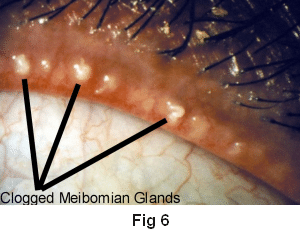 Meibomian Gland Dysfunction MGD refers specifically to functional abnormalities of the meibomian glands which could be resulting in inadequate or excess secretions from these glands, a change in quality of the secretions and or blockages that prevent proper lubrication of your eyes. Figure 3 above under Posterior Blepharitis shows the location of these glands and the picture here at Figure 6 shows and actual eye and blockages of the meibomian glands, one of the common symptoms.
Meibomian Gland Dysfunction MGD refers specifically to functional abnormalities of the meibomian glands which could be resulting in inadequate or excess secretions from these glands, a change in quality of the secretions and or blockages that prevent proper lubrication of your eyes. Figure 3 above under Posterior Blepharitis shows the location of these glands and the picture here at Figure 6 shows and actual eye and blockages of the meibomian glands, one of the common symptoms.
When functioning normally the Meibomian glands secrete a fine free-flowing transparent yellow oil (meibum) that ”floats’ on the tear film lubricating the eye and controls the evaporation of the tear film that protects your eyes.
If these glands are not producing sufficient oil, or if the oil becomes too thick and or blocks the outlet it can not only cause the immediate symptoms associated with blepharitis and MGD, but, if left untreated these blockages can result in permanent damage to the meibomian glands. This damage is a leading cause of dry eye syndrome.
It was reported in one study in Spain of 1155 subjects that nearly half the subjects with Dry Eye Syndrome had other associated diseases such as Pterygium, Glaucoma and Cataracts.
The takeaway here is for goodness sake get help if something is not right with anything to do with your eyes.
Treated early most problems can be contained if not cured.
Your eye sight is priceless, look after it.
Blepharitis and Dry Eye.
Once again we are faced with the question of which comes first, and there are a number of studies stating that blepharitis either causes or greatly exacerbates most cases of dry eye, with both being found together an many patients.
 There is essentially two types of dry eye syndrome one is called aqueous deficiency dry eye and as the name suggests this is caused by insufficient fluid being produced to keep your eyes from being properly moistened. Aqueous deficiency dry eye is usually brought about by a problem with the lacrimal glands which produce tears.
There is essentially two types of dry eye syndrome one is called aqueous deficiency dry eye and as the name suggests this is caused by insufficient fluid being produced to keep your eyes from being properly moistened. Aqueous deficiency dry eye is usually brought about by a problem with the lacrimal glands which produce tears.
The other cause more closely related to blepharitis and MGD is called evaporative dry eye. As mentioned earlier the meibomian glands normally secrete a fine oil which floats over the tear film on the surface of your eyes. This film of oil known as meibum prevents or slows the evaporation of the tear film and in the case of Meibomian Gland Dysfunction causing dry eye the oil film is either inadequate or too thick to do this job so the tear film quickly evaporates leaving the sufferer with uncomfortable dry eyes.
CHAPTER 3:
Is Blepharitis Contagious?
The answer to “Is Blepharitis Contagious” depends upon the type of blepharitis.
There are some eye infections labeled as blepharitis that are contagious. If it started suddenly, there is a high probability that is is contagious.
In this chapter we will look at contagious blepharitis conditions.
To find out if your blepharitis is contagious you need to see your doctor, ophthalmologist or optician .
Before your visit the doctor make a written list of your questions and concerns. When you are being examined it is easy to forget to ask.
Don’t feel intimidated it is your body, your eyes. The more information you can give the doctor the more able he or she can accurately diagnose the problem.
Asking questions will help you understand the problem and recommended treatment. This in turn will help you to follow treatment and manage your condition.
You do not want to come away from your appointment with more questions than answers.
Staphylococcal Blepharitis
 This form of blepharitis as the name would suggest is cause by staphylococcal bacteria, commonly known as “staph.” These bacteria are often present on our skin and in small numbers and do no harm.
This form of blepharitis as the name would suggest is cause by staphylococcal bacteria, commonly known as “staph.” These bacteria are often present on our skin and in small numbers and do no harm.
However there are many forms of this bacteria and in some people they can multiply causing infections of the eyelids leading to blepharitis.
Why this happens to some people and not others is not completely understood but, as with many diseases, poor health and or a compromised immune system can lay a person open to infections.
The onset of staphylococcal blepharitis can be quite sudden and is regarded as an acute condition. However left untreated in can lead to loss of eyelashes and the more intractable meibomian gland disease, so early diagnosis and treatment is important.
Another frequent and unwanted companion of these infections of the eyelid are Styes, Cysts, Chalazion and Pink eye which we will cover below.
While technically not blepharitis staphylococcal and viral infections of the eye are often referred to as blepharitis. I have included them in the study in case some patient has been given the diagnosis as Blepharitis and not fully understood the nature of these two infections.
Viral Blepharitis
 In appearance Viral Blepharitis can be very similar to Staphylococcal blepharitis and is also a contagious condition
In appearance Viral Blepharitis can be very similar to Staphylococcal blepharitis and is also a contagious condition
The example on the left was due to the herpes simplex virus infection. The eyelids become red and swollen with yellow crusts that emanate from small ulcers.
Often accompanied by conjunctivitis, resulting in inflammation of the membrane that covers the eye and the interior surface of the eyelids.
The herpes simplex eye infections which is the same virus that causes cold-sores are not generally serious and may persist for only a few days. However if left untreated some scarring can occur with the possibility of damage your vision.
While technically not blepharitis Viral Blepharitis and viral infections of the eye are often referred to as blepharitis. I have included them in the study in case some patient has been given the diagnosis as Blepharitis and not fully understood the nature of these two infections.
CHAPTER 4:
Blepharitis Treatment
Successful Blepharitis Treatment begins by knowing your enemy, Demodex mites.
In a recent study published in U.S. National Library of Medicine* Researchers found that: The incidence of Demodex infestation was 90% in cases of Anterior Blepharitis, 60% in Meibomian Gland Disease cases, and 90% in Mixed Blepharitis cases. The incidence of Demodex in people without Blepharitis was only 18%.
So if you have Blepharitis it is 90% certain you have a demodex infestation.
In this chapter we cover the various Blepharitis Treatments available. Accept for acute viral or bacterial blepharitis please keep in mind Demodex are most likely at the heart of the problem or at least part of the problem.
* National Center for Biotechnology Information, U.S. National Library of Medicine Ref PMC4219223

Acute Blepharitis
A sudden onset of Blepharitis is frequently caused by a Staphylococcal or Bacterial infection.
Treatment for bacterial blepharitis is the application of antibiotics by either ointment or eye drops. Ointments are favoured for children and drops for adults.
 Ideally a swab of the crusting and oil should be cultured to determine the type of bacteria before treatment as there are increasing instances of multi- antibiotic-resistant strains of staphylococci appearing and it is important to hit it with the right product.
Ideally a swab of the crusting and oil should be cultured to determine the type of bacteria before treatment as there are increasing instances of multi- antibiotic-resistant strains of staphylococci appearing and it is important to hit it with the right product.
A doctor or ophthalmologist is also likely to suggest an eyelids cleansing routine to ease the discomfort and assist in clearing it up.
Blepharitis caused by a Viral Infection may look similar to the above but it cannot be cured with antibiotics.
It is important to understand this difference as many people expect their doctor or ophthalmologist to prescribe antibiotics not realizing that they are totally ineffective against a virus.
Treatment in this case is usually cleansing the affected area and the use of eyedrops to ease the irritation and make it easier for the bodies own immune system to do the work.
A third but less common cause of these acute conditions is a fungal infection.
While technically neither of these acute infections are Blepharitis they are sometimes referred to under this broad heading.
Both infections are highly contagious and towels and Pillow (cases) should not be shared. They must be hot washed frequently separately from other items and preferably sun dried where possible. If you are only infected in one eye be careful not to spread it to the other eye when you wash an/or touch your face. And please, for the sake of others, avoid swimming in any public swimming pool.
They are more prevalent among children but in any case it is extremely important that you see a doctor and have the infection rapidly and correctly treated to prevent any potential permanent damage.
PLEASE NOTE: If you are not seeing rapid improvement when undergoing treatment or if it is still worsening, do not hesitate in returning to your doctor or seeking a second opinion. The picture above is from a gentleman who would have lost his eye if he had not been persistent in finding the right physician and treatment.
Treating Demodex Blepharitis
As many researchers have now established Demodex Mites are present and possibly the cause of many forms of Blepharitis. Whether demodex have caused your blepharitis or are just another aggravating component it makes sense to be rid of them.
The treatment for blepharitis caused by the demodex mites centres around a cleansing regime designed to kill the demodex mites and remove the irritating and infectious debris they create.
They have a lifecycle of between 14 and 18 days so it is important to establish a regimen that lasts for at least three life cycles of these critters. A rather unpleasant fact about demodex is that they have no anus so the content of what they have eaten is unloaded in your skin in one hit along with their rotting carcase at the end of their lifecycle.
It is believed that this a responsible for much of the allergic response and potential secondary infection they can cause.
To bring demodex mites under control a systematic eyelid cleansing regimen is essential. BlephroClear Eyelid Wash is very effective in doing this. Used night and morning to begin with it removes the unsightly crusting and flaking while killing the demodex mites. Six weeks of treatment will usually have you symptom free. This treatment involves the application of the eyewash cream to your eyelashes and lids twice a day and leaving it in place for 1 or 2 minutes before rinsing of with warm water.

Demodex mites are part of all of our lives and since you have developed blepharitis once you are probably more prone to reinfection so maintaining a regular hygiene routine of cleansing your lids and lashes several times per week with BlephroClear should prevent a reoccurrence. Ideally this can be done in the shower with the warm water also massaging your lids to begin and end the routine.
It may take a little discipline to continue after the symptoms have subsided but if you persist for a few more weeks it will become a natural habit that you won’t even have to think about. It is so worth it I promise you.
If you have had blepharitis for some time you have probably been prescribed lid scrubs with baby shampoo, warm compresses, and even steroid/antibiotic combo drops and more recently, topical or oral ivermectin.
Currently the treatments such as BlephroClear that have shown to be most effective in killing demodex mites are using tea-tree oil and or its active component Terpinen-4-OL. It has also been found that the water soluble components of tea-tree oil have an anti-inflammatory property which can also be helpful in treating blepharitis.
Note:
Baby shampoo is only helpful in removing some of the crusting but does nothing to cure the problem.
Steroids: Other than a very short term reduction of inflammation any steroids are better avoided as they can have very serious and permanent side effects with continued use. In a number of studies these products have been found to increase the inner eye pressure which can lead to Glaucoma.
Blepharitis is a Progressive Disease
 Regardless of whether you have had blepharitis for a short time or for several years it is extremely important to realise that blepharitis is a progressive disease/disorder and if left untreated it will only get worse.
Regardless of whether you have had blepharitis for a short time or for several years it is extremely important to realise that blepharitis is a progressive disease/disorder and if left untreated it will only get worse.
One of the biggest difficulties faced by clinicians is convincing their patients of the need to continue an eyelid cleansing regimen to reduce or eliminate the symptoms. And also that it is wise to continue that routine on a reduced basis after treatment rather than waiting for the likely return of the condition.
The video below gives you a close look at the problem
Ocular Rosacea
Ocular Rosacea could possibly be helped as well. I wanted to separate this from other forms of blepharitis because it is a much more complex condition and is just as likely to appear as a condition of the skin that does not have any symptoms affecting the tissue around the eyes.
 However when it comes to demodex mites the tie up with this form of blepharitis is dramatic.
However when it comes to demodex mites the tie up with this form of blepharitis is dramatic.
An adult with normal healthy skin has one or two demodex per square centimetre of skin on their face.
People with rosacea, however, can have as many as ten times that number.
Researchers believe that the cause of flare-ups of rosacea may be from a reaction to bacteria in the mite’s faeces which is released into the pores when they die and that this brings on an immune response causing inflammation and tissue damage.
Treating Meibomian Gland Dysfunction
There is literally hundreds of research papers, clinical studies and articles on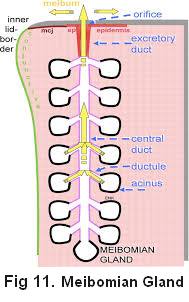 Meibomian Gland Dysfunction and its treatment. With the overwhelming amount of sometimes conflicting information available on this subject it has been quite a task to condense it down into a useful core of information.
Meibomian Gland Dysfunction and its treatment. With the overwhelming amount of sometimes conflicting information available on this subject it has been quite a task to condense it down into a useful core of information.
If you want more than I have provided in this or any other section of this site you will find an extensive bibliography and associated links in the last section.
To begin looking at the treatment options, let’s start with a few pictures so we can see exactly what we are up against.
This first graphic is a diagram of a single healthy meibomian gland on the lower eyelid.
The small bulbs “acinus” produce the meibum which travels up the duct to the orifice where it seeps out and provides a fine film of oil over the tear film. This layer of oil is instrumental in preventing evaporation of the tear film that lubricates and protects your eyes.
These glands can become blocked by many things such as dust particles or the scale from anterior blepharitis. Demodex infestations or various infections can cause the meibum to become thicker and when it ceases to flow this will gradually destroy the acinus bulbs and the gland will effectively die (called dropping out).
The aim of treatment is to restore the health of the meibomian glands by clearing the blockage and encouraging the production and flow of meibum before the glands drop out and, most importantly, maintaining this condition once this has been achieved.
Glands that have died cannot be restored which is why early intervention and an ongoing eyelid cleansing regimen is so important.
 Before looking at how the glands are unblocked, cleared and normal function restored there is something you really must understand.
Before looking at how the glands are unblocked, cleared and normal function restored there is something you really must understand.
These glands are sensitive and too much pressure or squeezing too frequently could destroy them. Also the production of meibum is a gradual ongoing process so squeezing them too often or too hard can empty them faster than the meibum is replaced. Then since there is insufficient meibum available to properly protect the tear film, you then find yourself suffering from more dry irritated eyes.
This can become a vicious circle with further squeezing leading to the empty glands becoming stuck together internally and ultimately dropping out.
Looking at the pictures above you can see the blocked glands and a massive amount of the semi congealed meibum. This is the excess that has built up in blocked glands which, if it continues to build up, eventually expands enough to destroy the gland(s).
Types of Treatment For MGD
It is best to get an experienced eye doctor to get the treatment process started an eye doctor will have the tools and experience to clear the blockages safely, usually over several visits progressively further apart.
LipiFlow Thermal Pulsation System
 Many doctors clear the glands manually with heat and gentle pressure but more recently a Thermal Pulsation System called LipiFlow has been developed which applies the heat and pressure much more precisely.
Many doctors clear the glands manually with heat and gentle pressure but more recently a Thermal Pulsation System called LipiFlow has been developed which applies the heat and pressure much more precisely.
It looks a little overwhelming but from the reports I have read it seems to be quite effective in getting patients over the difficult first stage of treatment, clearing the blockages and re-establishing a more normal flow of meibum.
In case this looks and sounds a little scary, here is a link to a youtube video showing LipiFlow in action. I think it will allay your fears.
Some further information is available here. evaluategroup.com
Footnote: The cost of the equipment and the disposable eye pieces high so this is a fairly expensive procedure.
The manufacturer Tear-Science has recently brought the cost of the disposables down to try and reduce the cost of treatment and you may also find quite a variation in price between practitioners depending upon where you live.
Yes you may only need this in the initial stage but shop around and dont be afraid to ask questions.
BlephEx Mechanical Eyelash Cleaning
There is a mechanical treatment available for cleaning the eyelids and eyelashes . This machine is called BlephEx and it is rather like going to the dentist to get your teeth cleaned.
. This machine is called BlephEx and it is rather like going to the dentist to get your teeth cleaned.
It is advertized quite widely but I found it difficult to obtain much independent research. I have read some good write-ups on the machine but I also know of several practitioners who were initially keen that have now ceased to use it.
I did however find one study that was published in Review of Ophthalmology that was quite encouraging. One comment that stood out to me was that it is particularly helpful for patients that find it difficult to establish or maintain a regular eyelid cleansing routine.
Some people who left comments after trying Blephex were not very happy with the results some reporting increased irritation. So if you are thinking of doing this I suggest doing some further research yourself and have a good chat with your eye doctor. You can download the study here
Blephex-study Review of Ophthalmology Oct 2015
Intense Pulse Light
IPL has been used successfully in treating MGD although it is a fairly specialized treatment and not  available in many places. A topical anesthetic is applied around the area to be treated, and an eye shield is used to protect the eye. It is a process similar (But not the same) as that used to remove unwanted hair or pigmentation.
available in many places. A topical anesthetic is applied around the area to be treated, and an eye shield is used to protect the eye. It is a process similar (But not the same) as that used to remove unwanted hair or pigmentation.
The effectiveness of the treatment appears to rely on two elements.
Like hot compresses, LipiFlow and other heat treatments, the heat generated by the IPL helps to melt the the meibum in blocked glands. They recommend expressing the meibomian glands immediately after IPL treatment.
The second element that IPL has going for it is that it has been shown that IPL does kill bacteria. Its use for blepharitis has stemmed from its success in reducing the effects of rosacea.
However on a cautionary note there is an inherent risk of eye damage when applying intense light (laser) in proximity to the eye.
BlephaSteam
BlephaSteam is another device that has been developed for home or clinical use that is designed to replace using a warm compresses. It delivers a moist heat at a constant safe controlled temperature to the eyelids to melt the coagulated meibum which can then be expressed with specifically designed forceps in the clinic or with gentle massage in the home environment.
use that is designed to replace using a warm compresses. It delivers a moist heat at a constant safe controlled temperature to the eyelids to melt the coagulated meibum which can then be expressed with specifically designed forceps in the clinic or with gentle massage in the home environment.
A good idea for those that can afford it. BlephaSteam
Blepharitis Home Treatment
Your focus should be on a daily hygiene routine for your eyes and eyelids including warm compresses and massage to keep the glands open and encourage them back into health.
Let’s look at this process in some detail beginning with a few important facts. You have no doubt read that warm compresses and massage are helpful in restoring normal function of these glands on the rim of your eyelids. But what is the right temperature? And how do you massage your eyelids correctly?
Normal body temperature is 37 Celsius (32.66 Fahrenheit) but this internal temperature and your eyelids can be much cooler. Meibomian secretions melt at 32◦C but since the meibum is thicker than it should be it will need a slightly higher temperature to melt. I suggest somewhere between 38 and 43°C.
Some will say as hot as you can stand but this is uncomfortable and unnecessary.
You may purchase reusable heat pads such as the ones produced by Quantum Heat Packs or use a thick clean washcloth soaked in hot water then rung out as much as possible. The advantage of the heat pads is convenience and better temperature control, the advantage of the washcloth is the warm moisture also helps to soften any matter clinging to your eyelids as well as the congealed meibum.
 Step 1. Apply the warm compress to your eyelids. Try and maintain the desired heat for around 15 minutes to open the pores and ensure the oils will flow easily.
Step 1. Apply the warm compress to your eyelids. Try and maintain the desired heat for around 15 minutes to open the pores and ensure the oils will flow easily.
Step 2. Remove the compress and immediately massage each eye (both upper and lower lids) for 5 minutes. Starting at the corner of your eyes closest to your nose, massage firmly but gently in a circular motion moving across your eyelid to the outer edge of your eyes.
Repeat the process starting at the outer edge and working in towards your nose. If necessary warm your eyelids again before the return run. Your vision may be a little blurry immediately after doing this as the thicker oil from the blocked glands is being released into your eyes.
Step 3. The last step is the essential cleansing of your eyelids and eyelashes with BlephroClear which not only cleans your eyelashes and prevents any debris and the expressed content from re-blocking the glands but is also healing and over time eliminates the scaling as well as killing any demodex which may have initiated the MGD in the beginning. Apply the eye-wash cream to your eyelashes and lids and leaving it in place for 1 or 2 minutes before rinsing of with warm water.
You should follow this routine every evening before going to bed for 5 or 6 weeks. If you have any sticky eyelashes in the morning repeat step 3.
The Importance of Maintenance
If you have been diligent with the above regimen you should be symptom free but regardless of how much better you may feel, some damage has been done and you are more susceptible to the problem reoccurring.
Knowing this, it is smart to establish a daily hygiene routine of massaging your lids and lashes and washing them with BlephroClear. This will keep the glands unblocked and the demodex at bay. Ideally this can be done in the shower with the warm water also massaging your lids to begin and end the routine.
It may take a little discipline to continue after the symptoms have subsided but if you persist for a few more weeks and just like cleaning your teeth it will become a natural habit that you won’t even have to think about.
but if you persist for a few more weeks and just like cleaning your teeth it will become a natural habit that you won’t even have to think about.
It is so worth it I promise you.
You would be well advised not to wear any eye makeup for the 6 week period and make sure you dispose of all previously used mascara, eye makeup and brushes to avoid recontamination.
CHAPTER 5:
Where To From Here?
I sincerely hope that this information has given you a good understanding of what you are facing with blepharitis and also the knowledge that with the right care, you can be free of it.
As you have seen every treatment method covered has also included an eyelid cleaning regimen to help in both eliminating the symptoms and maintaining healthy eyes thereafter.
I strongly recommend you try using BlephroClear. My eyes were an itchy irritated mess which I am happy to say is now two years in the past. BlephroClear is all I have used to achieve this.
I started by using BlephroClear twice daily and once my symptoms had largely subsided I reduced it to once a day and then only once or twice per week as a general hygiene routine.
While cleansing is central to regaining healthy eyes, lids and lashes I cannot emphasize enough the importance of seeing an eye-care professional to get your condition accurately assessed.
The bottom line is, your eyesight is precious and confidence in yourself and your appearance is difficult to maintain when you are constantly distracted by itching, burning eyes and embarrassed by how they look.
So see an eye care professional and get yourself on the road to recovery.
I wish you all the best
Raoul

Questions & Stories Welcome
Links & Studies on Blepharitis
General Discussion
- https://www.reviewofophthalmology.com/article/a-guide-for-breaking-down-blepharitis
- https://www.reviewofoptometry.com/article/getting-a-grip-on-blepharitis
- http://www.mayoclinic.org/diseases-conditions/blepharitis/basics/definition/con-20024605
- http://www.hopkinsmedicine.org/wilmer/conditions/blephartis.html
- https://www.dovepress.com/diagnosis-and-management-of-blepharitis
- http://optometrytimes.modernmedicine.com/optometrytimes/news/4-steps-beating-blepharitis
- http://www.spectator.co.uk/2016/10/save-your-sight-eight-vital-tips-for-better-eye-health/
- http://www.foxnews.com/health/2012/03/13/what-is-blepharitis.html
- http://mytoba.ca/life/health-fitness/dry-eyes-may-just-irritating/
Demodex
- ophthalmologytimes.modernmedicine.com/ophthalmologytimes/news/exploring-ocular-demodicosis-influence-chronic-blepharitis
- http://blogs.discovermagazine.com/notrocketscience/2012/08/31/everything-you-never-wanted-to-know-about-the-mites-that-eat-crawl-and-have-sex-on-your-face/#.WKEti_l95E
Studies
- https://www.dovepress.com/diagnosis-and-management-of-blepharitis-an-optometristrsquos-perspecti-peer-reviewed-article-OPTO
- ophthalmologytimes.modernmedicine.com/ophthalmologytimes/news/tea-tree-oil-proposed-blepharitis
- http://www.nature.com/eye/journal/v29/n12/full/eye2015144a.html
Makeup & Blepharitis
- http://www.thehealthsite.com/news/number-of-blepharitis-cases-rise-among-indian-women-experts-warn-against-usage-of-poor-quality-eye-makeup-ag0416/
- http://news.health.com/2015/11/13/best-mascaras-for-sensitive-eyes/
- http://www.empowher.com/eyes-amp-vision/content/protect-those-eyes-keep-healthy-makeup-bag
Computer use
- http://metro.co.uk/2016/04/14/do-you-work-on-a-computer-all-day-then-you-could-get-dry-eye-5817664/
- http://www.techtimes.com/articles/20235/20141114/prevent-against-eye-infections-contacts.htm
- http://home.bt.com/tech-gadgets/computing/computer-eye-strain-tips-for-healthy-eyes-11364052746654
Dry Eye
- http://mytoba.ca/life/health-fitness/dry-eyes-may-just-irritating/
- http://www.huffingtonpost.com/dr-boxer-wachler/9-surprising-treatments-t_b_5552453.html
Alternatives
Downloadable Blepharitis studies
- Blepharitis-and-lid-hygiene
- Blepharitis_v15 CLINICAL MANAGEMENT GUIDELINES
- Blepharitis_PPP
- Blepharitis_disease_and_its_management
- Blepharitis incidents and Treatment3607
- Blepharitis Ayuvedic 1463_pdf
- Blepharitis Anxiety and Depression
- Blepharitis and eyelid hygiene
- Blepharitis and Contacts Text.study_3355115
- Blepharitis – Fakten und Mythen
- ALPAFLORALP-SEBUMProductDataSheetv50615s
- The Epidemiology of Dry Eye Disease
- Seborrheic dermatitis
- Seborrheic Blepharitis
- Morbidity pattern of ocular
- July 2012 Clinical Update Cornea
- EyeLibrary-Blepharitis eye-conference
- Eye Health_MultiCultiCompanion_v08_
- Demodexf_TPD_409
- Common Signs, Symptoms, and Complications of Blepharitis
- Cholesterol Possible Association with Blepharitis
- Bunya_etal_13
- Blephex Study
- Blepharitis-Update-on-Research-and-Management
- Blepharitis-an-inflammatory-condition-of-the-eyelids Blephex Study


 Chapter 2
Chapter 2 Chapter 3
Chapter 3

